Abstract
Background: BMT CTN 0201 was a randomized trial of bone marrow (BM) vs. G-CSF mobilized blood (G-PB) grafts in 550 pediatric and adult patients with leukemia or MDS undergoing allogeneic hematopoietic stem cell transplantation from unrelated donors. Overall survival (OS) was equivalent between both arms, with more chronic graft-versus-host disease (GvHD) among recipients of G-PB grafts and more graft failure among recipients of BM grafts (Anasetti NEJM 2012; 367:1487-1496). We have previously reported donor plasmacytoid dendritic cell (pDC) content in BM grafts are linked with improved survival and less death from acute GvHD (Waller JCO 2014 32:2365-2372). Here, we compare the kinetics of immune cell reconstitution between BM and G-PB recipients to test the hypothesis that graft source leads to differences in blood levels of donor-derived immune cells, and that higher levels of dendritic cells are associated with lower GvHD-related death rates.
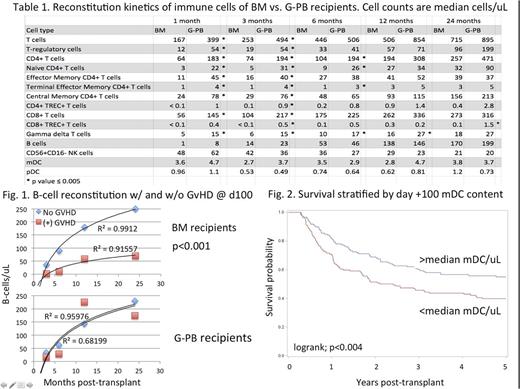
Methods: Demographics among randomized patients were similar with respect to diagnosis, conditioning regimens, GvHD prophylaxis, and CMV serostatus. Flow cytometry measured immune cells in blood samples at 1, 3, 6, 12, and 24 months post-transplant in recipients of BM (N=161) or G-PB (N=147) grafts from unrelated donors. Univariate and multivariable analyses evaluated associations between donor immune cells and outcomes.
Results: Reconstitution kinetics of immune cells at day +100 were associated with graft source, a history of GvHD, and subsequent GvHD-related death.
G-PB recipients had higher 1 and 3-month levels of blood T cells and B cells than BM recipients, as well as higher numbers of γ/δ, CD4+ T-reg, CD4+ T cells at later time points (Table 1). In contrast, recovery kinetics for pDC, mDC,and immature CD56+CD16- NK cellswere similar between each graft arm (Table 1). B cell reconstitution kinetics were slower in BM recipients, especially in BM recipients who developed acute GvHD prior to day +100 as opposed to those who did not (in Figure 1, p < .001). No significant association existed between aGvHD history and lymphocyte reconstitution in G-PB recipients.
Blood levels of immune cells at day +100 were associated both with a history of acute GvHD as well as subsequent 2-year OS, and GvHD-related death. All patients who developed grades 2-4 acute GvHD by day +100 had worse 2-year OS than non-GvHD patients (66% vs. 53%, p=.01). However, patients with a history of GvHD and >median numbers of blood mDC, CD4+, or CD8+ T cells at day +100 had better 2-year OS (95% CI): [mDC, 63 (51-74)% vs. 43 (32-55)% p=.02; CD4+ T cells, 64 (53-75)% vs. 42 (31-53)%, p=0.007; CD8+ T cells, 65 (54-76)% vs. 42 (31-53)%, p= 0.004] than GvHD-patients with <median numbers of these cells. Furthermore, significantly fewer GvHD-related deaths occurred in patients with >median numbers of mDC compared to in those with <median numbers of mDC (23% vs 40%, respectively, p<.05).
In contrast, G-PB recipients with >median numbers of blood central memory CD8+ (p=.01), CD8+ (p=.004), and γ/δ T cells (p=.002) by day +100 had significantly higher 2-year OS compared to those with <median numbers of these cells. BM recipients with >median numbers of mDC had higher 2-year OS compared to those with <median numbers (p=.06).
The content of blood mDC was prognostic for post-transplant outcomes for the entire cohort of patients and the subset of BM recipients. Significantly improved 2-year OS (95% CI) was observed in patients with >median numbers of mDC by day +100 post-transplant (68 (61-76)%) compared to those with <median numbers of mDC (51 (43-59)%; p=.008; Figure 2). Compared to the latter, the former also had significantly less (p=.04) treatment-related mortality at 2-years post-transplant (12 (8-18)% vs. 23 (17-31)%) and no difference in relapse (30 (23-38)%) vs. 29 (22-37)%).
Conclusions: Graft source is associated with differences in reconstitution kinetics of T and B cells. Blood levels of immune cells at day +100 are cellular bio-markers for both GvHD-related death and OS in transplant recipients, and are correlated with a history of acute GvHD. Specific cell subsets prognostic for OS vary by graft source. Higher levels of blood mDC at day +100 in BM recipients are associated with improved OS, while higher numbers of T-cells predict better OS in GPB recipients. Compared to BM recipients, G-PB recipients have faster T and B cell reconstitution as well as greater resiliency of lymphogenesis following acute GvHD.
Lee: Mallinckrodt: Honoraria; Amgen: Other: One-time advisory board member; Bristol-Myers-Squibb: Other: One-time advisory board member; Kadmon: Other: One-time advisory board member. Waller: Helocyte: Consultancy; Novartis Pharmaceuticals Corporation: Consultancy, Honoraria, Research Funding; Coulter Foundation: Research Funding; Katz Foundation: Research Funding; Chimerix: Equity Ownership; AMGEN: Consultancy; Cambium Medical Technologies: Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties; Celldex: Consultancy; Cerus: Equity Ownership; National Institutes of Health: Research Funding; PRA: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.